Clinical Mycobacteriology and Epidemiology (CLIME) Group
Projects

What is the feasibility, accuracy, and optimal manner in which next-generation tests for tuberculosis can be used in high burden settings? (The OPTIMAL DIAGNOSIS study)
This project is part of the EDCTP2 programme supported by the European Union (TMA2015SF-1041 The OPTIMAL DIAGNOSIS study).
Abstract
Tuberculosis kills ~1.4 million people annually and is a leading cause of death in sub-Saharan Africa. Sensitive and rapid point-of-care tests are expected to substantially reduce TB incidence and mortality, however, until recently, tests that meet these criteria are yet to become available. We propose a package of novel diagnostic studies to build local capacity and evaluate the feasibility, accuracy, and effectiveness of new, ultra-sensitive point-of-care tests for TB and drug-resistance in our high-burden, high HIV setting of Cape Town, South Africa.
Firstly, we will evaluate the accuracy and impact of Xpert Ultra (using the Omni system) and AlereQ TB testing for pulmonary TB at the point-of-care in clinics (n=360 patients). These tests, which likely have sensitivity equivalent to a culture, may have utility in patients with few or no symptoms (~1 in 5 TB cases are missed by screening algorithms). We will evaluate the utility of new screening tools, such as automated digital chest radiography, which may reduce costs and inform the optimal use and scale-up of new molecular tests.
In the second sub-study, we will, in collaboration with clinician-scientists, evaluate the accuracy and impact of Xpert Ultra and AlereQ TB for extra-pulmonary TB (pleural, cerebral spinal, and pericardial fluid; n=430 in total) compared to Xpert MTB/RIF at a major tertiary-level hospital, and examine whether they obviate the need for routinely performed tests.
In the third sub-study, we will evaluate the accuracy and impact (time-to-diagnosis, time-to-treatment) of next-generation tests (MTBDRsl v2.0, Xpert XDR) for second-line drug resistance on sputum, by accessing samples from a high throughput routine laboratory (n=960). Unlike current diagnostics for second-line resistance, these tests may be done directly on specimens, and thereby reduce patient attrition and delay associated with methods that require mycobacterial culture.
The fourth component is the creation of a well-characterised sample biobank from each sub-study (sputum, isolates, serum, urine, pleural fluid, cerebral spinal fluid, pericardial fluid) to serve as a platform for future research (e.g., evaluation of emerging diagnostic technologies, biomarker discovery) and student training. At least three postgraduate students will train as part of this project.
In addition to novel data on the accuracy and potential impact of new point-of-care tests for TB, this project will inform on how they can be optimally used (e.g., with automated digital chest radiography). This project addresses one of the most devastating poverty-associated diseases in Africa and has excellent fit with the objectives of EDCTP2.
Overarching goal:
To evaluate the point-of-care feasibility, accuracy and effectiveness of highly sensitive, next-generation diagnostics for the diagnosis of pulmonary TB, extra-pulmonary TB, and drug-resistant TB, whilst assembling a comprehensive, well-characterised biobank for the future research, training, and capacity development.
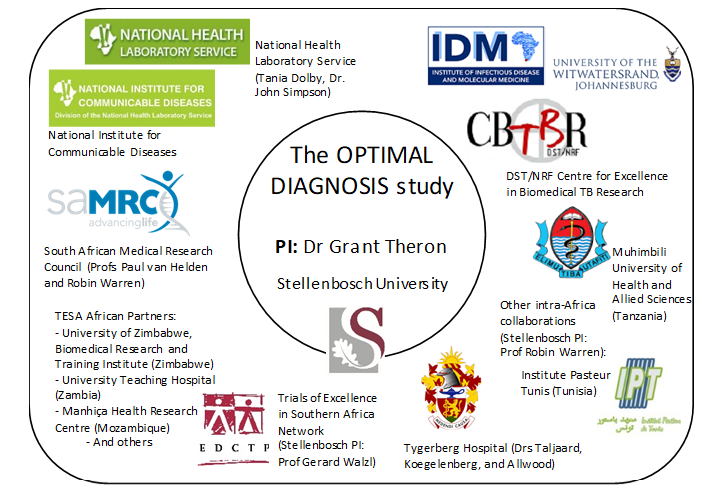
If you are interested in this project, please contact the PI (A/Prof Grant Theron,
gtheron@sun.ac.za). Outputs from this project are acknowledged and reported alongside others from the CLIME group
here.

