Clinical Mycobacteriology and Epidemiology (CLIME) Group
Projects

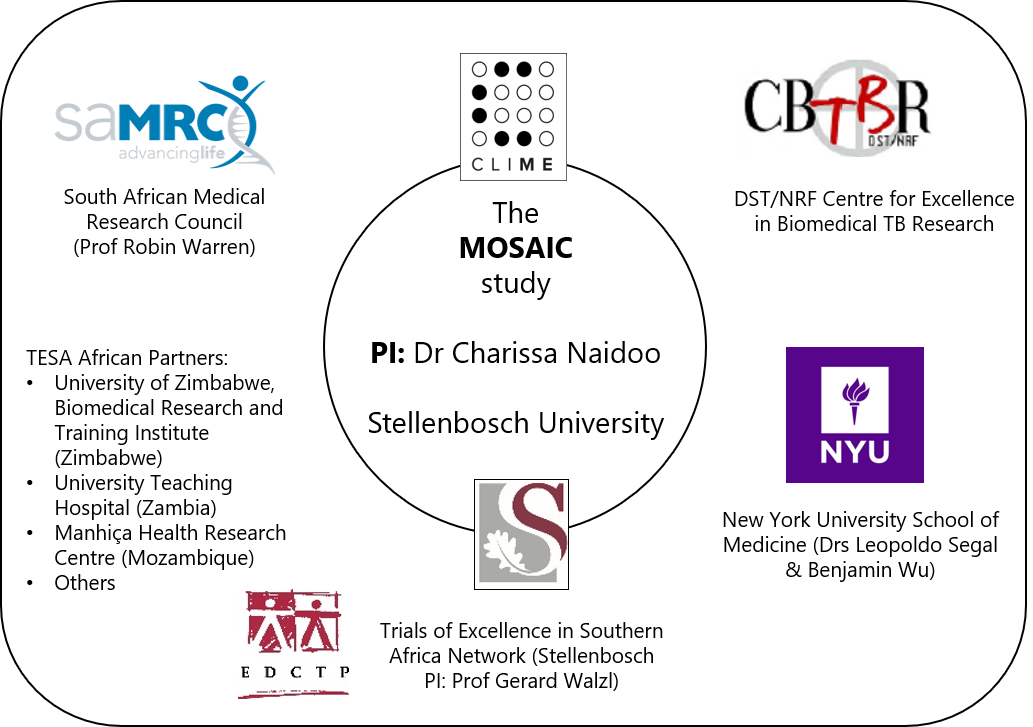
The longitudinal microbiome of South African tuberculosis patients, symptomatic culture-negative controls and healthy household contacts, and its association with treatment outcome (the MOSAIC study).
This project (TMA2017CDF-1914-MOSAIC) is part of the EDCTP2 program supported by the European Union
Abstract
Despite being readily curable, tuberculosis (TB) remains the single biggest infectious cause of death globally and, in South Africa, kills more people than any other condition. A large amount of TB is never diagnosed and, despite good adherence to treatment, a significant proportion of cases encounter unfavourable treatment outcomes (as high as ~20% in some settings). Hence, not only is there a need for better ways of diagnosing TB but novel methods of prognosticating patients likely to have unfavourable outcomes are needed. The microbiome (collection of microbial genetic material within a specific environment) is an emerging research area that has been implicated in disorders ranging from obesity to cystic fibrosis to survival in HIV-positive pneumonia patients, where it may be a therapeutic target. However, there are very little data in the context of TB. Capacity to study the intersection of TB and the microbiome is also limited in Africa.
In MOSAIC (Microbiome of South African Incident TB Cases), we propose to characterize the gut microbiome in 100 Xpert MTB/RIF-positive, culture-positive cases (pre-treatment, 2- and 6-months into treatment, and 6-, 12- and 18-months post-treatment), 50 matched symptomatic controls (Xpert-negative, culture-negative), and 200 healthy household contacts (two per case; culture-negative) in Cape Town, South Africa. We will leverage a SAMRC funded project (BAR-TB) recruiting patients with presumptive TB, performing testing (Xpert, culture), microbiological and clinical follow-up. In MOSAIC, we will, in addition to the work in BAR-TB, collect microbiome specimens, recruit and collect the same specimens from healthy contacts. We are an international multidisciplinary team comprised of a young TB researcher with emerging experience in computational biology (the candidate), mycobacteriologists and diagnosticians (Warren and Theron), pulmonologists with experience in the microbiome and lung disease (Segal and Wu), and immunologists (Walzl).
The application includes 1) long-term support for a post-doctoral fellow, 2) development of her scientific, management and mentorship skills (she will co-support trainees), 3) the enhancement of local computational biology capacity, and 4) the collection of additional specimens for future microbiome research (e.g., host transcriptomic correlates). Hence, the application has a high likelihood of resulting in advances regarding the role of the microbiome in TB that may, in the long-term, lead to targeting of the microbiome for diagnosis or treatment outcome. It also includes capacity development aspects that will enable the candidate to begin to transition to an independent research position with expertise in a new and neglected research area in Africa.
Overarching goal
To evaluate the association of the microbiome with active TB (pre-treatment culture-positive patients vs. symptomatic culture-negatives vs. healthy household contacts), treatment, and treatment outcome.
If you are interested in this project, please contact the PI (Dr Charissa Naidoo, ccnaidoo@sun.ac.za). Outputs from this project are acknowledged and reported alongside others from the CLIME group here.

