Clinical Mycobacteriology and Epidemiology (CLIME) Group
Projects

The influence of tuberculosis treatment on the emergence of antimicrobial resistance amongst the ESKAPE bacteria (The ESKAPE-TB study).
Abstract
Globally, the emergence of antimicrobial resistance (AMR) due to antibiotic usage is considered one of the most pressing future health problems. Tuberculosis (TB), which kills more people worldwide than any other infectious disease, requires hundreds-to-thousands of doses of antibiotics to achieve cure. Remarkably, the impact of TB treatment on the emergence of AMR within the residential microbial flora in the human body has not been investigated. If TB treatment causes AMR, it may have significant implications there is hardly any data on combating AMR.
Perhaps the most important group of bacteria involved in AMR in humans are the ESKAPE bacteria
(Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and
Enterobacter spp). These are important residents in our bodies but cause most drug-resistant opportunistic infections, especially in critically ill and immunocompromised individuals, such as HIV-positive individuals. In this study, we will evaluate longitudinally the impact of 6 months of standard TB treatment and the longer drug resistant TB treatment on ESKAPE AMR emergence within the gut microbiome.
The proposed study aims to first quantify the relative abundances and associated antimicrobial resistance genes before, during, and after TB treatment (first- and second-line treatment). In addition to microbiomic taxonomic sequencing, we will use an innovative targeted multiplex sequencing assay to detect resistance in major carbapenemase genes, plasmid-mediated quinolone resistance determinants,
gyrA and
parC chromosomal genes, several aminoglycoside resistance genes, trimethoprim-sulfamethoxazole, tetracycline, streptomycin, chloramphenicol, and fosfomycin resistance genes, and the recently discovered plasmid-mediated colistin resistance gene
mcr-1 in each of the ESKAPE taxa. We hypothesize that the ESKAPE bacteria increase in relative abundance during TB treatment and this increase is associated with AMR. This research will provide insight on the proposed impact of TB treatment on the gut microbiota resistome which has not been investigated. This will lay the foundation for potential interventions to limit AMR emergence and carriage during TB treatment; thereby protecting invaluable antibiotics, including those used for conditions other than only TB (e.g., fluroquinolones). This application includes 1) salary support for a post-doctoral fellow, 2) support for scientific mentorship skill development, 3) enhancement of capacity building and computational biology expertise of Sub-Saharan Africa.
Overarching goal
To evaluate whether an increase in the ESKAPE bacteria and AMR occurs during TB treatment (first- and second-line treatment).
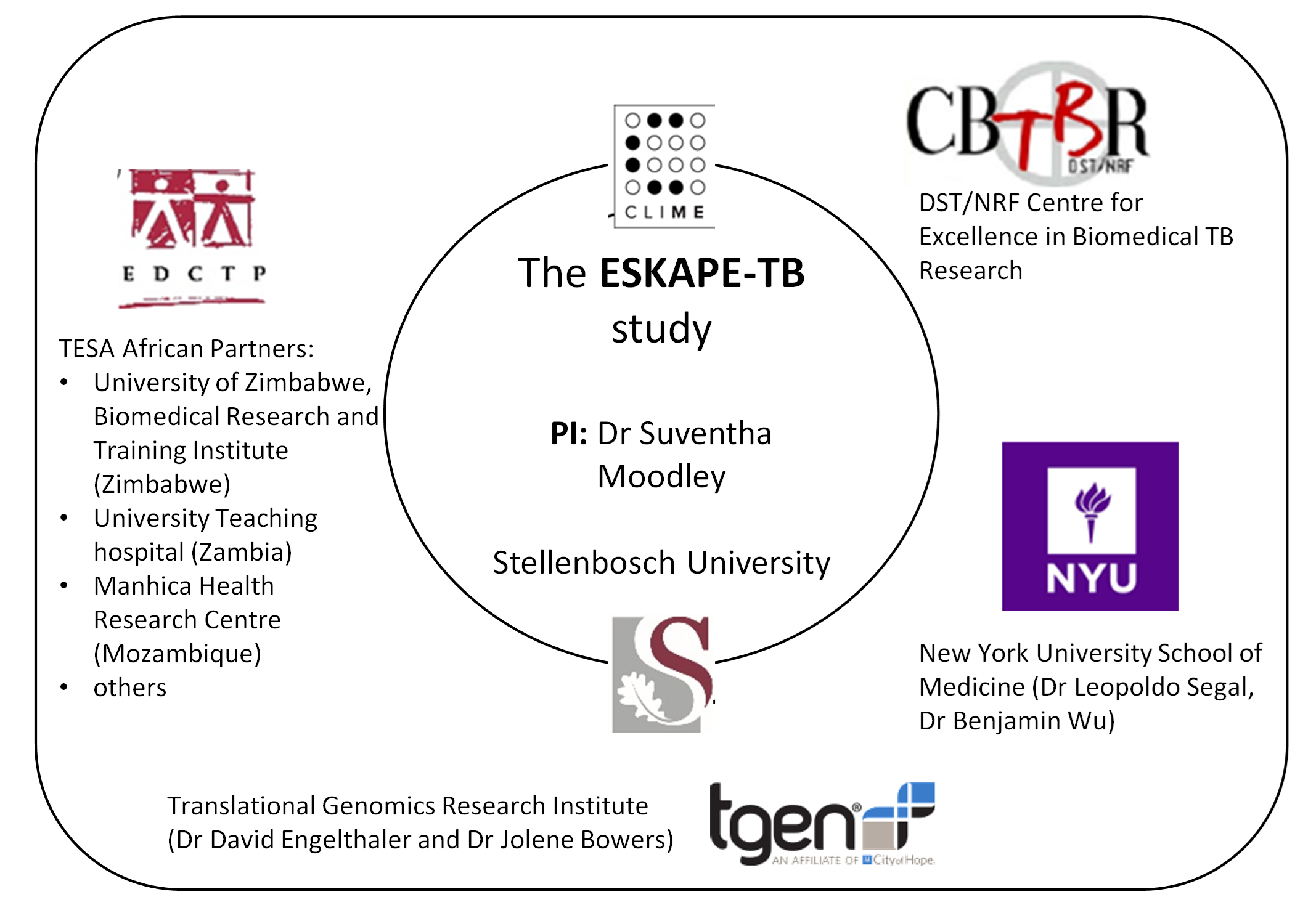
If you are interested in this project, please contact the PI (Dr Suventha Moodley,
suventha@sun.ac.za).

